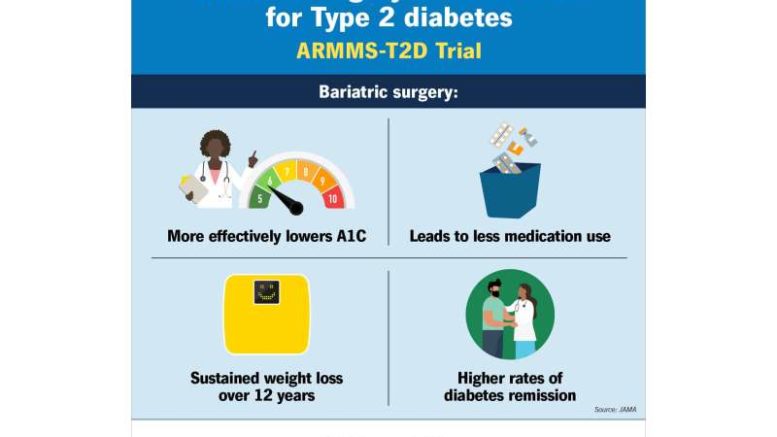
New research led by a surgeon-scientist from the University of Pittsburgh School of Medicine, published in JAMA, suggests that bariatric surgery is significantly more effective than medical and lifestyle modifications in achieving long-term control and remission of type 2 diabetes.
This study, described as the largest and longest randomized follow-up study to date, indicates that bariatric surgery not only improves diabetes control and remission but also leads to more effective management of cholesterol and triglyceride levels compared to conventional interventions. Given the impact of diabetes and cholesterol on heart disease risk, these findings suggest potential benefits in reducing cardiovascular complications.
Lead author Dr. Anita Courcoulas stated, “This analysis is the strongest evidence we have to date that bariatric surgery is a safe and effective tool for achieving diabetes control and remission.”
The research involved comparing outcomes such as blood sugar control, weight loss, and medication usage among participants enrolled in four separate randomized clinical trials conducted between 2007 and 2013. Patients with type 2 diabetes and obesity were assigned either to undergo bariatric surgery or to participate in a medical and lifestyle program focused on established interventions for diabetes risk reduction. Data from these trials were pooled for analysis, with long-term outcomes assessed at seven and, where possible, 12 years post-randomization.
Results indicated that patients in the bariatric surgery group consistently exhibited lower HbA1c levels, indicative of improved blood sugar control, compared to the medical/lifestyle group at each follow-up point. At year seven, 18.2% of surgery group participants achieved diabetes remission, compared to 6.2% in the medical/lifestyle group. By year 12, no patients in the medical/lifestyle group were in remission, while 12.7% in the surgery group achieved remission.
These benefits were observed across different weight class groups, suggesting that bariatric surgery is equally beneficial for patients regardless of BMI. Dr. Courcoulas emphasized the importance of offering bariatric surgery as a treatment option for inadequately controlled diabetes, even for patients below the typical BMI threshold for surgery solely for weight loss.
Although the study primarily focused on diabetes outcomes, it also highlighted the superior durable weight loss achieved through bariatric surgery compared to medical/lifestyle interventions. However, there were no significant differences in mortality or major cardiovascular events between the two groups, although adverse effects such as anemia, fractures, and gastrointestinal symptoms were more common in the surgery group.
The study utilized data from randomized clinical trials conducted at various institutions, emphasizing the robustness of the findings across diverse settings. Overall, the results underscore the potential of bariatric surgery as an effective treatment strategy for type 2 diabetes, supporting the need for individualized and flexible care approaches based on patients’ health conditions and goals.